by Beverly Bernstein Joie, MS, CMC, Aging Life Care Association™ Member
One Professional’s Personal Experience with Medicare Observation Status
My husband, Dan, came home from work on December 23, 2014 and, as is our fashion, I asked him about his day. When he began talking, It was evident he could not find the words to tell me about it. We were both perplexed. Then he hit me with another bit of news, “When I read my emails, I can’t see the whole sentence. There are pieces that are missing.” My heart immediately dropped!
As a Certified Care Manager and an Aging Life Care™ expert, I knew something was not right. We jumped into the car and I drove frantically to the ER. After a cardiogram revealed no heart attack, the relevant CT scan and MRI were ordered. We began the three-hour wait to see the doctor. Based upon a prior stroke (CVA) seven months earlier and his current symptoms, the doctor’s assumption was that he had a mini-stroke or “Transient Ischemic Attack (TIA).”
The testing revealed “no change” but TIA’s do not typically show up on testing. His prior stroke had affected the Basal Ganglia area of his brain. Symptoms such asaphasia (word finding difficulty) and the organization of speech are associated with this type of stroke and many others. An overnight stay at the hospital was no surprise. After waiting until 10 PM for a bed, Dan suggested I go home and come back in the morning.
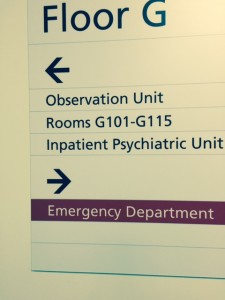
When I arrived the next day, the hospital case manager greeted me. She proceeded to tell me that my husband was “under observation.” Instantly, my role transitioned from caring wife to assertive Aging Life Care™ Manager and advocate. I demanded my husband’s status be changed to “in-patient.” There is no way he understood any forms he may have signed after I left the hospital the night before.
Shortly thereafter, the orders for a discharge were signed, sealed, and delivered. I, however, was not going anywhere unless I had a document in hand that proved my husband was an in-patient. His primary nurse let us know she was leaving for lunch, to which I responded that without the document of in-patient status printed out, she would be spending her lunch time with us. She agreed that if we left the hospital without documentation, we would never see it.
Why the Fuss Over Observation Status?
While observation status is nothing new; the recent abuse of observation status is. Recently, Medicare recipients who require a hospital stay are being placed under observation status rather than admitted as an in-patient, with the explanation that doctors need time to evaluate the patient’s status.
Here’s what you need to know about Observation Status:
- Outpatient services and Observation Status are billed under Medicare Part B; inpatient services are billed under Medicare Part A.
- Medicare Part A pays for hospital charges. There is also a deductible – $1,260 per benefit period in 2015.
- Medicare Part B requires patients to pay 20% of the cost. There is no cap on total expenditures.
- Observation patients pay out-of-pocket for their medication received in the hospital. If they have Medicare Part D, they may be reimbursed IF their Part D formulary includes the medications they receive.
- If patients require post-acute services in a skilled nursing facility, it is not covered unless they are an in-patient and have remained an in-patient for three consecutive nights. No observation status patient can receive this benefit.
The Centers for Medicare & Medicaid Services (CMS) established the Readmissions Reduction Program under the Affordable Care Act and added section 1886(q) to the Social Security Act as of October 1, 2012. As a result, Medicare recipients who return to the hospital within 30 days of an inpatient stay for the same diagnosis force hospitals to incur a financial penalization for this readmission.
Observation status patients are not considered inpatients. Consequently, they have never been admitted into the hospital. The use of this criteria means that hospitals will not be penalized if the patient returns in less than 30 days. This serves the hospital well, but could compromise the patient financially and eliminate an opportunity for rehabilitation services due to the prohibitive cost of such care.
Postscript
Dan is doing well. The neurologist suspects the TIA diagnosis was incorrect based upon Dan’s symptoms and his observation of Dan’s status. The neurologist believes the symptoms were from a more benign cause.
As for me, I often think of those unsuspecting patients in the Observation Unit of hospitals. I wonder how they will feel when the bills start coming in; or even worse when they are unable to receive rehabilitative services. I wish everyone had an Aging Life Care Manager who could educate them and advocate for their health care while also protecting their pocketbook! To find an Aging Life Care Expert near you, visit aginglifecare.org.
About the author: Beverly Bernstein Joie, MS, CMC, is President of Complete Care Strategies in King of Prussia, PA. She can be reached atbbjoie@completecarestrategies.com.